Bioethics Tool Kit
- meganjungers
- Feb 9, 2025
- 3 min read
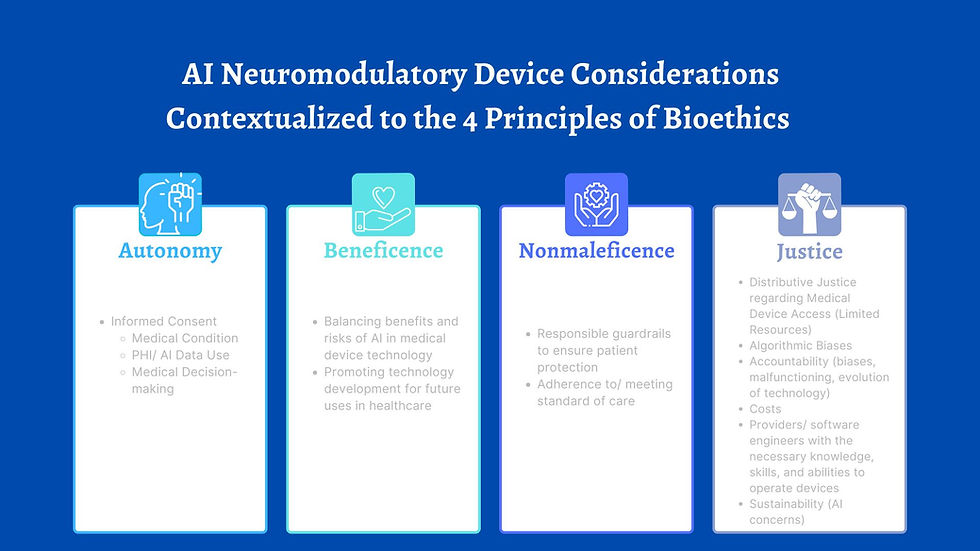
There are an array of weighted considerations within the bioethics space to include in the discussion of the potential benefits and risks of using neuromodulatory medical technology devices with AI components. In order to best facilitate our discussion, we want to offer a "Bioethics Tool Kit" in order to establish operational definitions for some terms and concepts we will be using in future blog posts, but also to make sure that we are working with the same technical bioethical backgrounds for our discussions.
The four key items to familiarize yourself with in this context are the 4 Principles of Bioethics as popularized by Bioethicists Beauchamp and Childress1 :
Autonomy in this context, specifically relates to when "they are made intentionally, free from controlling influences and with adequate understanding of medically-relevant information." 2 In this sense, we are looking specifically at patients (or, individuals in the market) having access to all the information available about:
1) Their condition.
2) A comprehensive understanding of the different risks and benefits of the medical device intervention.
3) What could potentially happen with the data they would be providing to the artificial intelligence inside the medical device.
With answers to each devices regarding this outlined criteria we can assess if a patient's autonomy is respected in the process of determining their respective course of treatment with a medical device.
Beneficence relates to taking action to promote the most good for a patient. This principle is particularly of importance with weighing conventional standard of care practices with novel, technologically-dependent devices that have less long-term use research. The pace at which technology and research is being introduced to support care practices is unprecedented, and the balance between providing patients with new treatment options and standard "best" care are valuable factors when assessing what care would promote the most good.
Nonmaleficence is a principle synonymous with the intent to "do no harm." In contrast to beneficence, this guiding principle articulates the intent to inflict minimal pain and suffering to the patient. There are varying degrees of potential harm associated with each type of medical device; some are more invasive than others, while some incorporate complex software. When we are weighing the principle of nonmaleficence in our decision to use a medical device for treatment purposes, the potential risk of harm is a important factor to contextualize.
Justice as a guiding principle aims to consider the many elements of fairness and access with regard to treatment. Medical device technologies are associated with unprecedented justice concerns, as the standard of care is evolving at an exponentially rapid pace. Further, there are often limitations associated with the number of these devices available, the costs of using and maintaining their functionality, and who is responsible for accounting for biases within artificial intelligence algorithms. Justice aims to answer the question of how do we provide each patient with respect for "each [they are] due." 3
We recognize that there are many different interpretations/ definitions of these terms, however within the context of this platform, we want to use the terms and concepts as described above.
Citations
Tom L. Beauchamp, and James F. Childress. 2013. Principles of Biomedical Ethics. New York, Oxford University Press. https://www.allisonkrilethornton.com/wp-content/uploads/Medical_Ethics_Readings/BandC-Moral-Dilemmas.pdf
Lewis, Jonathan, and Søren Holm. 2022. “Patient Autonomy, Clinical Decision Making, and the Phenomenological Reduction.” Medicine, Health Care, and Philosophy 25, (4): 615–27. https://doi.org/10.1007/s11019-022-10102-2.
Zalta, Edward N., ed. 2023. "Justice." The Stanford Encyclopedia of Philosophy (Fall 2023 Edition). https://plato.stanford.edu/entries/justice/.




Comments